

(Not all alveoli participate in gas exchange at a given time, resulting in some shunting.) In acutely ill patients, especially those on mechanical ventilators, pronounced changes in ventilation and/or perfusion may occur, causing a much greater disparity between arterial and end-tidal values. Circulating blood CO 2 is slightly greater than exhaled CO 2 due to a ventilation-perfusion (.V/Q) mismatch.

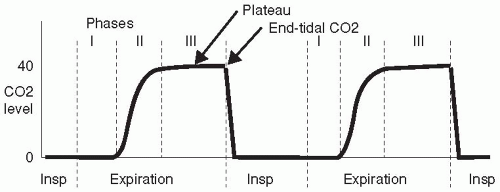
In patients with normal pulmonary function, CO 2 (normally 35 to 45 mm Hg) and ETco 2 should correlate closely, with a deviation of about 2 to 5 mm Hg. Ventilation/perfusion matchingĮTco 2 reflects metabolism, circulation, and ventilation. Because inspired air has negligible CO 2 amounts (less than 0.04%), exhaled CO 2 can be monitored and used as a correlate to assess CO 2 gas exchange and effective ventilation.

As a result, oxygen from the alveolus (where Po 2 is about 100 mm Hg) diffuses into the blood, and CO 2 diffuses from the blood into the alveolus (where Pco 2 measures about 40 mm Hg). In the pulmonary artery, deoxygenated blood has a partial pressure of carbon dioxide (Pco 2) of approximately 46 mm Hg and a partial pressure of oxygen (Po 2) of roughly 40 mm Hg. Gases diffuse from areas of higher concentrations to areas of lower concentration. The lungs serve as a pump to promote the activity of ventilation. This process occurs in red blood cells, where HCO 3– is released back into the plasma ready to accept another hydrogen ion (H+), while CO 2 and H 2O are carried to the arterial-alveolar junction for release into the atmosphere. While ETco 2 monitoring doesn’t directly indicate acid-base balance, it can shed light on ventilation efficacy.ĬO 2 combines with water to create H 2CO 3, which can degrade to bicarbonate, water, and CO 2. Both pH and CO 2 are measured from arterial blood gas (ABG) samples. As HCO 3-, CO 2 influences blood pH direct CO 2 measurement indicates ventilatory effectiveness. Depending on blood pH at any given time, CO 2 converts either to carbonic acid (H 2CO 3, an acid) or to bicarbonate (HCO 3-, a base).ĬO 2 exists in three primary states in the blood: as HCO 3– (70%), bound to hemoglobin (20%), and dissolved in the plasma (10%). CO 2 plays an important role in acid–base buffering. Cells take in oxygen and glucose and release water, carbon dioxide, and energy. The science behind the techniqueĬO 2 is a byproduct of cellular metabolism. Keep in mind that ETco 2 findings are interpreted within the context of physical and other traditional assessment methods. Although ETco 2 is used in non-intubated patients, here we focus on its use in patients with endotracheal intubation. This article explains these concepts, discusses ETco 2 waveforms, and describes the assessment capabilities of this monitoring method. To fully optimize its use, clinicians must understand certain basic principles. Although the principles underlying ETco 2 monitoring have been known for many years, recent technological advances have made the technique feasible for routine clinical application. Wherever ETco 2 monitoring is used, it can enhance patient safety-as long as bedside clinicians understand the interplay among ventilation, perfusion, and CO 2 production. Author Guidelines and Manuscript Submission.


 0 kommentar(er)
0 kommentar(er)
